When you’re in a loving, committed relationship, having a baby should be the most natural thing in the world. Yet one in six couples in the UK are affected by the devastation and pain fertility issues wreak.
Today sees the start of #YouAreNotAlone Fertility Week. Run by the charity Fertility Network UK, the main focus is to spread awareness for fertility issues to a wider audience.
Infertility is a condition of the reproductive system in either partner, or a combination of both, that prevents the conception of children; the diagnosis of infertility is usually given to couples who have been attempting to conceive for at least a year without success.
Dealing with infertility packs a massive emotional punch and can take its toll on relationships. #YouAreNotAlone Fertility Week will provide support on many levels, from sharing tips from mental health experts and outlining your rights as an employee to educating young people about lifestyle factors that could affect fertility, and highlighting the male voice from men facing infertility.
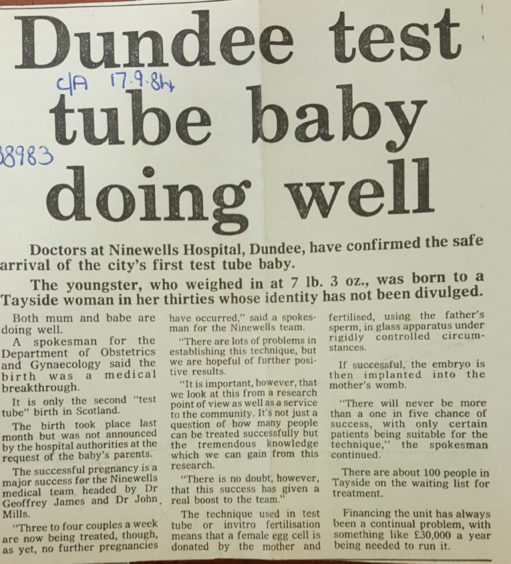
The Assisted Conception Unit (ACU) at Ninewells Hospital in Dundee has been carrying out treatment since the early 1980s when Drs John Mills and Geoff James established the unit and developed it into one of the largest centres in Scotland, opening in its present location in Ward 35 in 1994.
Ellen Drew, lead clinical embryologist at ACU and head of the andrology service, has been interested in IVF since the birth of ‘test tube baby’ Louise Brown in 1978. While studying for A Levels, Ellen attended an evening lecture by obstetrician and IVF pioneer Patrick Steptoe. An Honours year course in embryology included two lectures on IVF and an interest became a passion…
“Being unable to conceive naturally can be very difficult and all-consuming for couples,” she says.
Once patients have met the required criteria for NHS funding, which includes unexplained infertility of at least two years’ duration, being in a stable relationship for a minimum of two years and both partners non-smoking for at least three months, up to three cycles of a number of treatments can be considered depending on the circumstances – IVF (in vitro fertilisation, where the eggs are fertilised by sperm in the laboratory; ICSI (the treatment for severe male factor infertility when sperm is injected in to the egg; sperm retrieval; frozen embryo transfer; and ovulation induction.
“We do approximately 400 fresh cycles per year, and these are 55% IVF and 45% ICSI,” Ellen explains.
“We also do approximately 275 frozen embryo transfer cycles.
“Success rates always fluctuate, and are different in different age groups and whether a patient has one or two embryos transferred. More than one embryos transferred increases the risk of a twin pregnancy, which brings many health risks, and is to be avoided where possible,” she continues.

“IVF has approximately 45% clinical pregnancy rate while ICSI around 40% clinical pregnancy rate.
“With frozen embryo transfer the embryo survival rate is approximately 98% – which is brilliant – and clinical pregnancy rate of around 50%.
“All four NHS centres (Glasgow, Aberdeen, Edinburgh and our unit) are very generously supported by Scottish Government and we have the best patient funding in the UK.”
Consultant obstetrician Sarah Martins da Silva – recently named on the BBC’s 100 Women 2019 list has an active research programme focused around male infertility, sperm biology and drug discovery.
“The Assisted Conception Unit at Ninewells is a world-leading research enterprise offering evidence-based and protocol-driven care, embedded in a desire for continuous research,” Sarah says.
“We have a fertility counsellor within the unit, and we’re also affiliated with fertility groups, but dealing with all the emotional and physical implications of infertility can be such a difficult and lonely and frustrating journey and that’s why #YouAreNotAlone is such an important message.
“Information is very important but even our information is limited – there’s so much more that we don’t yet know about and that’s what makes research so vital.
“Assisted conception treatments are wonderful but not 100% guaranteed – it’s an imperfect science so it can be a difficult conversation,” she continues.
“I try to be realistic with people and not set expectations too high and offer false hope.”
Courtney Spears received ovulation induction treatment at Ninewells and is now 20 weeks pregnant.
“Being unable to conceive was isolating and confusing and I was aware that time was slowly passing by,” Courtney recalls.
“Nobody in my family had had similar problems and all my friend and colleagues were having babies so there wasn’t anyone I could really talk to before my referral to the unit.
“The support my partner and I received at the unit was fantastic – they explained every part of the treatment in way we could understand, and also made it feel very personal to us. All the staff have been amazing and we wouldn’t be in this position without them.”
It was a long and difficult journey for Kimberley McGill and her partner that finally resulted in a healthy baby girl, now three and a half.
“As a same sex couple the treatment was a step forward for us and very exciting,” recalls Kimberley.
Over the course of a year, she underwent three rounds of IUI (intrauterine insemination) unsuccessfully, followed by two rounds of hormone medicated IUI, which were also unsuccessful.
“I had a couple of tests which revealed issues that were making conception difficult so the next step was IVF,” she says. To the couple’s delight, the first round of IVF was successful and Kimberley can’t thank the unit enough.
“We felt so supported by everyone and so comfortable there – it felt like we got to know the staff as friends.”
Info
The ACU is always grateful for egg and sperm donors. If you’d like to find out more, please email tay-uhb.acureferrals@nhs.net