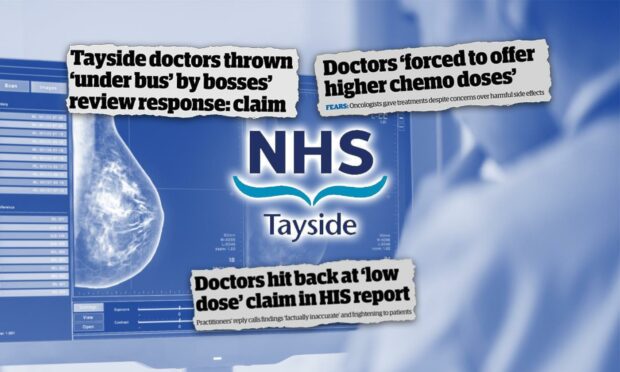
It has been almost three years since we first learned that nearly 200 breast cancer patients were given “lower than standard” doses of chemotherapy drugs by doctors at NHS Tayside.
The aftermath of that revelation has seen the region’s breast oncology service thrown into turmoil and patients forced to travel to other health board areas for their care.
Every single doctor who accused bosses of throwing them “under the bus” over the row has now left.
Despite multiple ignored requests for meetings with two different health secretaries and the first minister, patients and families have been left without answers.
Our reporting on the breast cancer scandal, which you can access in full here, has uncovered a litany of botched government reports, missed opportunities and accusations of a cover-up.
Here is everything we know so far.
When did the problems in NHS Tayside begin?
Patients in Tayside were given lower doses of chemotherapy drugs compared to other Scottish health boards between December 2016 and March 2019.
An independent review to fully consider the findings found patients should be fully informed of any variation in their care from generally accepted guidelines.

However, HIS first discovered two years earlier that no regional guidelines on dosing had been agreed in the north of Scotland for breast cancer chemotherapy, and that none had existed for a number of years.
The doctors claim there is no clinical risk to the lower dose and that the higher dose would be “unacceptably toxic” for their patients.
They also say the higher dose specified by other health boards was not always adhered to for this reason and that the lower dose was as effective in saving lives.
What impact did the lower chemo doses have on patients?
The benefits of chemotherapy drugs in terms of survival rates is a hotly-disputed topic.
A risk assessment ordered by the chief medical officer stated patients given the lower dose were put at a 1-2% increased risk of having their cancer return.
The review group behind the assessment concluded the treatment regime was “outwith best current practice and close to being unacceptable”.
NHS Tayside accepted these findings in full and began taking “immediate action” in response, including offering the stronger dose to every patient.
Why are the findings disputed?
Dr David Dunlop, who chaired the review group, admitted the increased risk figure was not based on specific evidence but rather “on the expert judgement of leading cancer specialists based on clinical experience built up over many years”.
Dr Greg Wilson, a leading specialist at the Christie Hospital in Manchester, was among the first to openly question the findings.
He dismissed as “absolute rubbish” any suggestion the increased risk figure could apply to a general patient population, many of whom he said would not be able to tolerate a higher dose.
Then professor Mark Chaplain, who specialises in analysing mathematical models of cancer growth at St Andrews University, insisted there are international studies to back up claims that lower doses do not cause increased harm to patients.
He called for a national review to find definitive answers for patients and families.
We later uncovered that another specialist behind the risk report privately admitted the findings were “flawed, probably, but the best that could be done really”.
In correspondence seen by The Courier, professor David Cameron outlined how the review group “assumed a roughly linear benefit” of providing higher doses, despite not being certain if this was correct.
Dr Dunlop later stepped down from his role as Scotland’s senior medical officer for oncology after being suspended by his own health board in an unrelated matter.
Why was a further review scrapped?
The Royal College of Physicians London was invited to conduct a review of breast cancer services but this was later scrapped due to a conflict of interest.
An initial feedback report completed in late May 2019 was shared with NHS Tayside management and the then-chief medical officer.
It is understood the full review would have been critical of the handling of the revelations by management at NHS Tayside.
The conflict of interest related to the involvement Dr Adrian Harnett, a specialist who was also recruited as an external advisor by NHS Tayside in 2017 for an internal investigation after the dosing revelations first came to light.
Dr Harnett also previously worked with a senior member of the oncology team as part of a research group on treatment guidelines and was further involved in supporting the Tayside oncologists following the publication of subsequent reports.
The Scottish Government faced criticism after being warned of the conflict of interest in April 2019, weeks before the initial feedback was submitted and months before the report was scrapped that October.
Dr Harnett later voluntarily removed his name from the medical register after being reprimanded by the General Medical Council (GMC) over the undeclared conflict of interest.
Who else has been investigated?
We revealed in November that those investigations effectively cleared individual team members over use of the doses and found the clinicians involved behaved appropriately despite not telling patients about the practice.
The GMC noted the outcomes of using lower doses “have largely not been compared in clinical trials and therefore cannot be said to offer proven inferior outcomes”.
It added it “would not be normal practice for an individual consultant to discuss with a given patient the differences in chemotherapy doses recommended or the other possible regimens available either in their centre or at another centre”.
NHS Tayside said it would not comment on the report as it is a “confidential matter between the individual doctor, their regulatory body and the individual who made the referral” to the GMC.
How has the breast cancer scandal escalated?
The breast oncology scandal has led to an exodus of staff and the associated reputational damage has made it difficult for NHS Tayside to recruit new consultants.
This has been compounded by a national shortage of breast cancer specialists.
Health chiefs have been forced to send some patients to Aberdeen, Glasgow and Edinburgh for treatment and could face further issues when Tayside loses its final breast cancer consultant later this year.
Meanwhile, the breast cancer scandal within the health board shows no signs of disappearing.
There have been multiple calls for an independent inquiry, most recently from the co-conveners of the Scottish Parliament’s cross-party cancer group.
We revealed in December how freshly uncovered correspondence shows health chiefs and government officials were given multiple direct warnings that reviews into the scandal were “deeply flawed” and would lead to the breast oncology service collapsing.
The health board also finds itself at the centre of bombshell cover-up claims.
He is said to have described their behaviour as “on a par with those actions reported in respect of the most major public life scandals of the last 20 years”.
Dr Pratt alleges the health board’s “own medical management” privately accepts there is no clinical evidence patients were put at any increased risk – but have allowed doctors to remain in the firing line.
More than a year later, Dr Pratt is still seeking answers for doctors and patients.
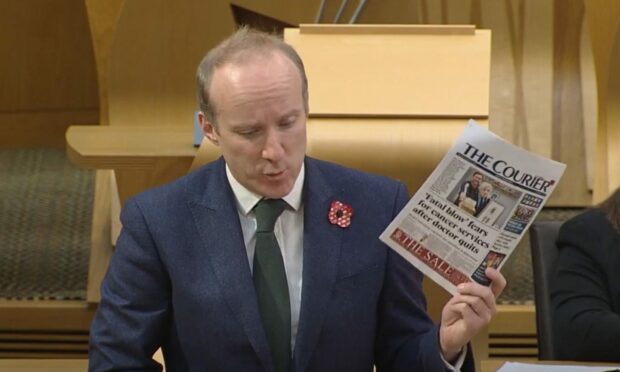
What have our leading politicians said?
The first minister has repeatedly been urged to step in and secure the future of breast cancer treatment in Dundee.
Ms Sturgeon said: “I certainly want to see breast cancer services have a long-term future in Dundee. That, I’m sure, everyone in Dundee wants to see.”
But in November her deputy, John Swinney, was accused of putting his own constituents in Perthshire North at risk by “burying his head in sand”.
Asked about what has been done since Ms Sturgeon’s pledge to tackle staffing issues in February, Mr Swinney pointed to the recruitment of a consultant – who has now also handed in his resignation.
He added that he hoped that would provide “reassurance” to members of the public in Tayside.
Mr Yousaf said: “Medical directors have been in contact with several of the larger cancer centres in England who are reporting similar challenges.
“So yes, we will absolutely work closely with Tayside. It is, of course, a deeply regrettable situation that they are in.
“It is not unique to Tayside, it is felt acutely in Tayside, but it is a wider issue.”