For three weeks, Mike Higgins fought the ventilator that was pushing oxygen into his Covid-inflamed lungs with such ferocity that he was given a heavy dose of drugs to tolerate it.
High levels of muscle relaxants were needed to paralyse him while sedatives and opioids dampened his agitation.
Even after coming out of the 21-day coma, the maths teacher from Kirkcaldy struggled badly with the life-saving medics who tried to keep him intubated in a coma.
When he was brought out of the coma, he was convinced that the Intensive Care Unit (ICU) team was trying to kill him – he even warned his wife Jill of this belief.
‘Some people fear falling asleep at night’
The terrors of the treatment vital to survive Covid were almost as painful for some patients, he explains.
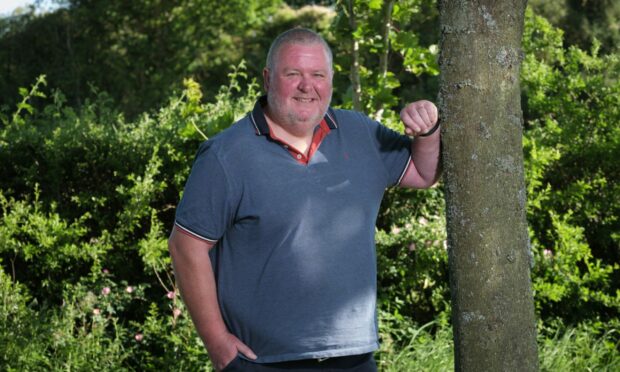
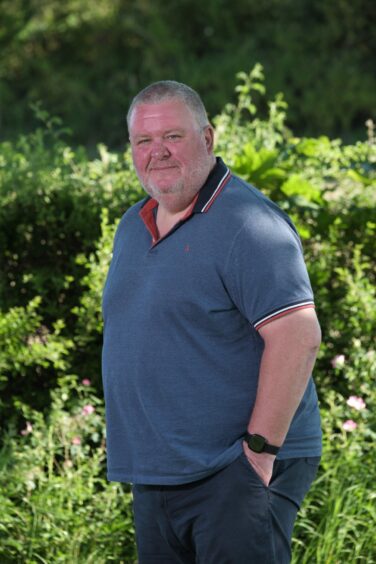
Today, 18 months after almost losing his life, Mike, 55, heads up a group of ICU patients who are trying to overcome those lasting effects of anxiety, post-traumatic stress and depression.
Doctors say that a third of patients who endure the rigours of ICU emerge with serious mental health problems.
And the burden of Covid has driven that number up hugely, medics add.
“Some patients are having nightmares so bad, they fear falling asleep at night,” Mike says.
“Thankfully, I don’t and sleep much better, but I am acutely aware of what others are struggling to endure. Bad dreams include being held down and feeling strangled by that vital breathing equipment.”
The heavy duty drugs necessary to help patients tolerate intubation also play terrible tricks on the mind, he says.
“I emerged fearing that the staff were going to murder me, and it was a while before ICU doctors and nurses could reassure me that I was safe.
“The noises of the machines keeping me alive fed into my hallucinations. The drugs needed in ICU can seriously affect your judgment as you work to recover.
“Some former ICU patients have suffered badly. My hallucinations included being captured by terrorists. I also thought I had died and watched my own funeral.”
‘Someone had to die for me to get a bed’
Regardless of the impact of intensive-care drugs, he is forever grateful to have been admitted to the Victoria Hospital, Kirkcaldy.
“I won’t forget that someone had to die for me to get a bed in ICU at Covid’s peak. Despite everything the medics could do, 15 had died before me.”
The dad of two heads up the patient group in Fife – one of five that have emerged in Scotland to help those traumatised by ICU. They have been developed with the support of nationwide patient groups run by charity ICU Steps.
Those who have recovered in ICU before Covid now head up the other groups in Edinburgh, Kilmarnock, Paisley and Dundee.
Post-traumatic stress disorder
Former intensive care nurse Pam Ramsay, a senior lecturer at Dundee University’s school of health sciences, has been a driving force and reveals that 30% of people who endure ICU treatment emerge with post-traumatic stress disorder (PTSD).
Ramsay said: “The numbers of patients who underwent intensive care for Covid has driven numbers up. Some have been frightened to fall asleep for years because of the nightmares about being in induced comas necessary to save their lives.
“These patient-led groups have recently been awarded £187,000 funding as part of the Scottish Government’s Covid recovery programme.”
Others helping guide the patient groups include George Guy, chair of the Edinburgh group, who underwent ICU after major surgery for oesophageal cancer seven years ago.
Just in excess of 20% of people who suffer oesophageal cancer are alive five years later.
“I needed to give something back by helping others who have survived life-threatening illnesses,” he says.
“We have worked closely with superb support from the Scottish Recovery Network, a Scottish mental health group with longstanding expertise in developing peer support resources and training.”
Mental health needs
Dr Nadine Cossette, liaison psychiatrist, at Royal Infirmary Edinburgh, was commissioned to examine mental health needs of patients admitted to hospital with Covid.
Cossette reported that severe Covid often continued after patients left hospital, with up to a third developing serious mental health problems, including PTSD, depression, anxiety, cognitive problems (memory, concentration and reasoning).
Given the huge scale of the Covid pandemic, this has increased the burden on Scotland’s mental health services, she adds.
The impact on families is also considerable, says Mike’s wife Jill Higgins.
‘I kept much of it from our teenage children’
“Like the many parents whose partners fought to survive Covid in ICU, I kept much of it from our two teenage children.
“We were unable to visit Mike. Not even when doctors called to say they were turning him on his front as a last-ditch attempt to save his life. It allowed more oxygen into his lungs.
“When he emerged thinking staff were killing him, I feared what the future might hold. Mike has recovered and back in the teaching job he loves, now desperately keen to help others.”
Meanwhile, Thomasina Brown, says being a member of the ICU patients support group at Crosshouse Hospital in Kilmarnock has played a vital part in her recovery.
“Doctors and nurses performed no less than a miracle when they saved me,” she says.
The grandmother 58, from Kilmarnock known affectionately as Tommy to her family, became desperately ill from Covid which was to kill her sister, brother-in-law and make another sister seriously ill.
She had been working as a carer when she became sick in November 2021 and, after a week in hospital, spiralled into ICU to fight for her life.
“When doctors transferred me into the ward where my brother-in-law died, I knew I had to do everything possible to survive,” she adds.
Armoury of antibiotics to survive Covid
She speaks as a member of the support group for patients at Crosshouse Hospital who are recovering from the long-term effects of intensive care. They are being guided by previous survivors who fought sepsis, major viral infections and other major illnesses in ICU before the pandemic struck.
“My sister died, and my own breathing deteriorated after being taken to hospital,” she says.
“Within a week of being admitted I had to be put into an induced coma to survive. I was to spend 72 days in a coma – in and out of consciousness – fighting Covid and a serious infection that threatened to overwhelm me.”
An armoury of the strongest antibiotics was needed for her to survive.
“Staff called my husband Billy several times daily with updates,” she says. “I was turned on my front to give my lungs every possible chance to work.”
At home her husband and three sons were primed for the next phone update, willing her to survive.
Families were often not allowed into ICU because of the risk to them.
Eventually, when she improved enough to be brought out of the coma, she found she could not feed or dress herself and struggled to make even basic moves. Her right arm and hand are still damaged by the effect of Covid.
“During the coma my grandson was born, as life went on for my family. One of the first things I remember as I brought back was that we were expecting a new grandchild,” she says.
‘Weird and wonderful nightmares’
It was a reach for normal that was to prove a turning point.
However, not being able hold her new grandson was distressing. “I had gone from being a carer to someone who needed cared for, and losing independence is difficult to accept,” she says.
Now, Brown says, the patient groups are a godsend. “Above all, the life-saving care in ICU and rehabilitation have helped me survive.
“Fortunately, staff keep diaries for ICU patients that help piece together what they have been through.
“I had both weird and wonderful nightmares where I dreamt that I had died but refused to accept it because I needed to get back to my family.”
- This article originally appeared in the print edition of The Sunday Post on June 25 2023