Perthshire grandmother Liz Mason enjoyed climbing Munros, going skiing in the winter and horse-riding every week until one morning she woke up and found she could hardly breathe.
The 81-year-old, who lives in Blairgowrie, assumed she had caught an infection.
“I remember it was in July 2013 and I had been climbing Munros that week,” she says.
“And this one morning I woke up and discovered I couldn’t breathe.
“I had been up coughing and wheezing through the night and I actually thought at one stage I was going to have a heart attack.
“I went to the doctor’s and was given antibiotics as it was thought I just had an infection.
“But it didn’t clear it.”
It turned out the retired independent junior school owner had developed Bronchiectasis.
It is a long-term condition where the airways of the lungs become widened.
This can then lead to a build-up of excess mucus which can make the lungs more vulnerable to infection.
While there is currently no cure, there are some treatments which can help prevent further damage and infections, and reduce symptoms.
Today Liz, who was diagnosed with Bronchiectasis ten years ago, refuses to let the condition hold her back.
Since the diagnosis she continues to be active – she has even climbed a Munro!
She also hopes new treatments will be found – particularly given recent news that Dundee researchers have identified the world’s first potential therapy for Bronchiectasis.
Diagnosed with Bronchiectasis
In the summer of 2013, when Liz first went to her local doctor’s surgery in Blairgowrie struggling to breathe, she was given antibiotics.
“The doctor thought I just had an infection,” she says.
“But the first lot of antibiotics didn’t work so I went back and I was given another lot.
“Over the course of the next three months I had three lots of antibiotics.
“But I continued coughing and was struggling to breathe properly. This went on for weeks.
“Eventually I called the doctor and told her I needed to be seen by a specialist.
“I said I had been up every night coughing my lungs up and these antibiotics were doing nothing.”
Liz was referred to Ninewells Hospital and secured an appointment in January 2014.
She then was given various tests including a spirometry test and tests for allergies.
Spirometry is the most common type of pulmonary function or breathing test.
It measures how much air you can breathe in and out of your lungs, as well as how easily and fast you can the blow the air out of your lungs.
“Nothing serious came out of these tests and so I pushed to get a lung scan.
“I remember the specialist looking at me and saying: ‘I don’t think you will find anything more in a scan.’
“However, I had the scan and two or three weeks later guess what? The results showed I had Bronchiectasis and that’s when I was formally diagnosed.”
No cure for Bronchiectasis
The first question Liz asked the specialist at Ninewells Hospital is when she would be clear of the condition.
“I asked how long will it be until I get this clear? At that point I was six months out of my hiking and I was anxious to get back to it.
“And I will never forget his response.
“He said: ‘You will never get rid of it’.
“I was quite shocked when he said that. I had been very fit and active and so this turned my life around.”
Liz, who is a non-smoker, isn’t sure how she developed the condition.
“They don’t know what caused this nor why I was susceptible to it.
“I have had pneumonia twice, although it was decades ago, which could have weakened my lungs, but it also could have been a virus.”
She was given antibiotics and steroids to treat Bronchiectasis initially.
But it took a number of years until she found the correct medication to help her manage the condition.
Liz continues: “Every morning I wake up with mucus which I need to clear from my lungs.
“I have to do this with specific breathing exercises – inhaling by nose and exhaling from mouth to expel the mucus/ phlegm.
“It’s long and tiring but if lungs are clearer and free from phlegm, the antibiotics reach the infected lungs better.
“I take antibiotics for flare ups in bronchiectasis. There is also a specific antibiotic I take three times a week is to reduce inflammation in my airway.”
Before developing Bronchiectasis
Liz, who owned and ran independent junior school Sea View in Kirkcaldy for 22 years, has always been very active throughout her life.
“I was super fit and had always loved horse-riding and hiking.
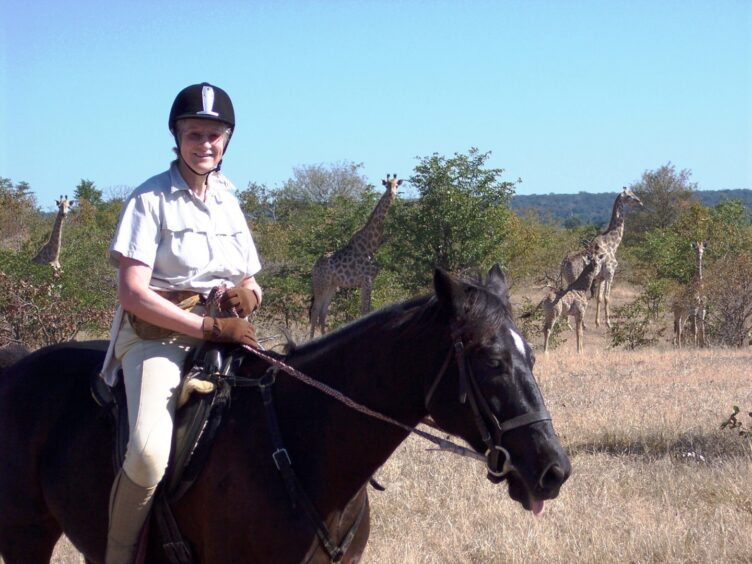
“I used to hire horses from local horse-riding schools or when on horse-riding holidays in America, Africa, and Canada.”
Liz also joined a hiking club after she retired and this was when she started climbing Munros in earnest when she was in her 60s!
She says: “I was one of the fastest hikers in our group – I could walk fast and climb fast – and I really enjoyed it.
“But after I developed Bronchiectasis, I had to stop it all because I was finding it too difficult to breathe while climbing.”
However, over the course of the last few years, Liz has been able to get back to doing some of the activities she loves – after finding the right medication to manage her condition.
Support from family
She has also had support in dealing with her condition from her three daughters Jackie, who lives in Perth, Rhona, who lives in America, and Fiona, who stays in Edinburgh.
This has included family outings, hill-walking and climbing a Munro!
“I was determined to do some of the things I enjoyed doing before I was diagnosed with Bronchiectasis,” Liz says.
“One of my daughters, Fiona, who lives in Edinburgh, is a hiker and three years ago, she suggested climbing one of the Munros at Glenshee and so we both did it together.
“I just have to take my time these days because I am a bit slower now.
“But I am determined not to give up.”
Liz also still enjoys travelling abroad, which she has done for many years, particularly to America where her middle daughter Rhona lives with her husband Jason and their four children, Callum, 25; Aidan, 23, Logan, 21 and Keira, 17.
And just in March this year she enjoyed a holiday in the Caribbean with Rhona and grandchildren.
Hope for new treatments
Liz is hopeful that new treatments will be developed and that a cure for Bronchiectasis will be discovered one day.
It follows recent news that Dundee researchers have identified the world’s first potential therapy for the chronic lung condition.
At the start of this month, Insmed, a biopharmaceutical company, announced promising results from its Phase 3 ASPEN study.
The study revealed that patients treated with a new investigational therapy, brensocatib, had significantly fewer lung flare-ups.
The University of Dundee, a leading research centre for bronchiectasis, has been at the forefront of the research.
Insmed plans to seek regulatory approval for brensocatib, aiming for availability by mid-2025 in the U.S. and 2026 in Europe.
The breakthrough offers new hope to millions of bronchiectasis patients, like Liz, who are awaiting effective treatment.
She says: “I think this new treatment is absolutely phenomenal and you should always have hope through life.
“I think this is a positive step forward for people who are affected by this condition.”
She added: “I am determined to keep going and to live past the age of 90 if I can – if my lungs keep working!”
Anyone with a lung condition needing support can contact the Asthma and Lung UK charity’s helpline on 0300 222 5800.
















Conversation