For generations it has seemed that a visit to the hospital or to a GP to discuss an ailment will end in the same manner – with a prescription.
They remain a lifesaver for many, but increasingly there is a realisation that the NHS needs to shift away from such traditional thinking for both financial and medical reasons.

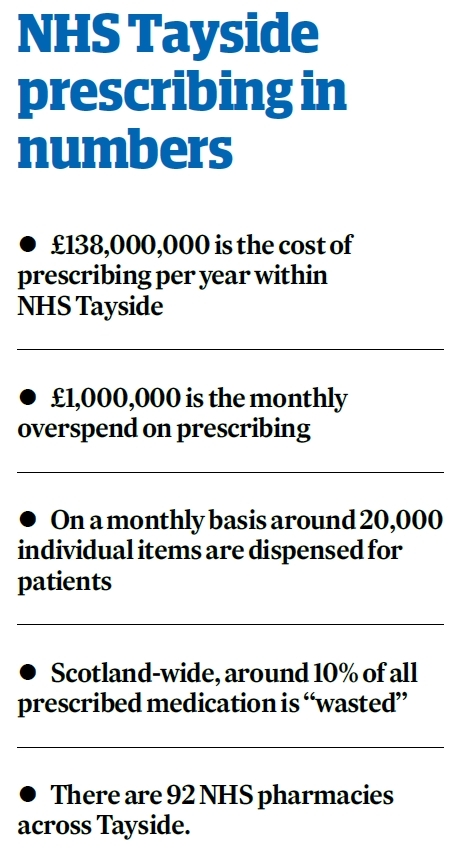
Prescription drugs are one of the health board’s biggest financial outlays, at £138 million annually, and the issue is reaching a critical tipping point with the monthly overspend now more than £1m.
In addition, it is estimated as much as 10% of all drugs prescribed across Scotland are never used and simply consigned to the back of a cupboard or the waste bin.
Within Tayside, that represents an average of £1.4m per year wasted on unused medicines.
Even more importantly, as the population grows older, an increasing number of the region’s patients are suffering from multiple ailments and take a cocktail of drugs.
Clinicians are increasingly aware that this can have a catastrophic effect upon the health of patients, with adverse drug reactions now linked to as much as 10% of all hospital admissions.
As a result, they are looking to reduce unnecessary prescribing as a matter of urgency.
That will require a concerted effort, a shift in thinking from GPs, doctors and nurses, and a significant shift in attitudes from patients towards their care.
Director of pharmacy Frances Rooney and associate director of pharmacy David Coulson have been tasked with leading that transformation.
Mr Coulson said: “We know that traditionally people like to leave their GP or hospital with something in their hand.
“They feel that medicine will make them feel better, but that is not always the case.
“We need to assure ourselves that we are using medicines that add values to patients and we need to challenge why we prescribe certain things.
“There can be other solutions that will make things better.”
Managing the delivery of thousands of prescriptions each week is a huge operation, key to which is the state-of-the-art robotic pharmacy at Ninewells Hospital, Dundee.
It was one of the first of its kind in Scotland when introduced in 2010 and remains at the forefront of dispensing technology.
Row upon row of pharmaceuticals, from paracetamol and mouthwash to life-saving drugs, sit side by side, while a secure area contains hundreds of specialist substances.
Using a conveyer belt and a bank of computers, a small army of staff stock the robotic pharmacy with countless individual drugs.
Its four linked robots fill shelves and then select prescriptions to be sent out to hospitals, surgeries, health centres and patients across Tayside.
While many of those drugs play a vital role in improving and maintaining the health of people across the region, others are simply wasted.
Ms Rooney and Mr Coulson will be at the forefront of efforts to reduce that massive waste bill and the untenable annual cost of prescribing.
Ms Rooney said it was important that the public help to reduce waste, thinking about what they actually need, discussing prescriptions with GPs and working to avoid stockpiling.
“We see the number of yellow bins that every community pharmacy has and they come back full to the brim with wasted medicines every month,” she said.
“Sometimes patients or carers order repeat prescriptions they don’t really need and stockpile them at home.
“The money that is wasted could be redirected into front line staffing and other much-needed health services.
“We are passionate about getting people involved and taking on board these key messages. If they help us, then there will be benefits for everyone.”