A patient at Ninewells Hospital died after being given a do not resuscitate (DNR) order despite family members claiming they did not authorise it.
A watchdog has told NHS Tayside to apologise to the family concerned for “record keeping” errors.
The mistake meant conversations about putting in place the DNR were not recorded and the health board’s documents did not show any disagreement by the family at the time.
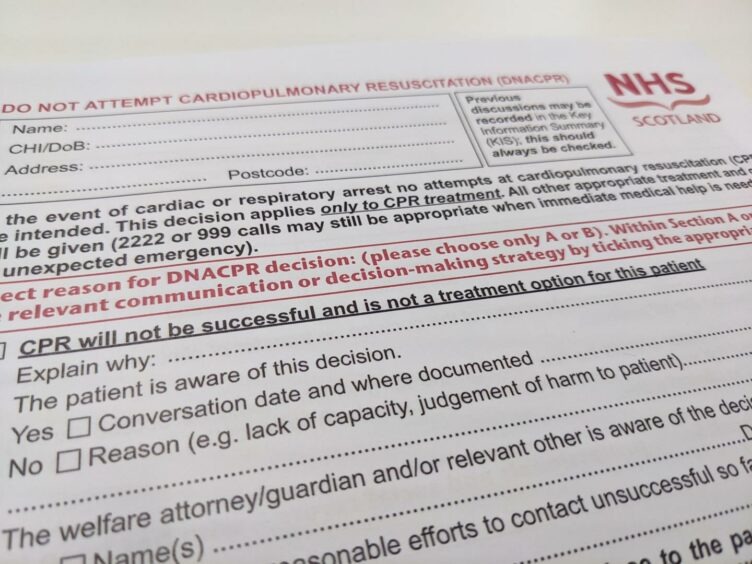
A DNR is a decision taken that means a healthcare professional is not required to resuscitate the patient if their heart or breathing stops.
In an investigation into the situation, the Scottish Public Services Ombudsman (SPSO) found the family believed the decision to grant a DNR order was taken “incorrectly”.
The report does not say what caused the patient’s death, or if resuscitation could have prevented it.
The ombudsman also found the form was only signed by one clinician, rather than the two required, and ordered the health board to ensure it always documents conversations about DNRs.
Decision could have ‘massive implications’
The error has been criticised by Dundee siblings Catriona Black and Rod McKay, who have been calling on stricter controls over DNR use after they found a form “stuffed inside” their mother’s bag when she was discharged from Ninewells in May last year.
She said the decision by the SPSO in this latest case could lead to further hospital deaths being investigated.
She said: “I am not the least bit surprised by it.
“But I am pleased this case was upheld and hope it focuses minds on the legitimacy of what happens to frail, vulnerable, disabled and incapacitated members of our society.
“The finding has massive implications going forward.
“As we now know, what happened to mum and this other person in Ninewells were not isolated — or even a regional occurrence — they were widespread throughout Scotland and indeed the UK.”
DNR use questioned
DNR use became a huge topic of controversy last year at the height of the pandemic.
It emerged patients across the UK, particularly the elderly, felt pressured into signing the forms, which are designed to prevent potentially harmful or futile CPR.
Some meanwhile are believed to have had such an order applied without their permission or their families’ permission.
Last year, The Courier reported on one of the first situations to came to light when an 86-year-old from Dundee agreed to her GP surgery’s “do not resuscitate” request despite suffering memory problems.
It left the elderly patient’s family in complete shock with daughter Helen Wray hitting out at the GP.
Call for review of DNRs
The Scottish Government has always maintained there has been “absolutely no change” in the use of DNR forms during the pandemic in the Scottish NHS and no change in advice on their use to GPs.
But Ms Black says there should now be a review of every DNR order to ensure all have been applied with permission.
She said: “I personally know many DNRs still sit in patients’ files.
“Can these patients have them revisited and reviewed?”
The SPSO’s ruling states: “We found that the board failed to follow appropriate processes and procedures in relation to the implementation of the DNACPR [do not attempt CPR], in as far as they failed to both adequately document conversations with family members, and to complete the required paperwork correctly.
“Clinicians involved should reflect on the complaint and identified failures with respect to the implementation of the DNACPR, specifically documenting communications with family and completing the relevant paperwork and forms.
“Medical professionals and clinicians are aware of, and adhere to, relevant professional standards and guidance with respect to maintaining clinical records and recording decision-making.”
A spokesperson for NHS Tayside said: “We accept all of the recommendations and have already apologised to the family.
“We are working to address the remaining recommendations.”