A Fife widow has issued an impassioned plea to save Dunfermline’s hospice, saying she would never have coped without it.
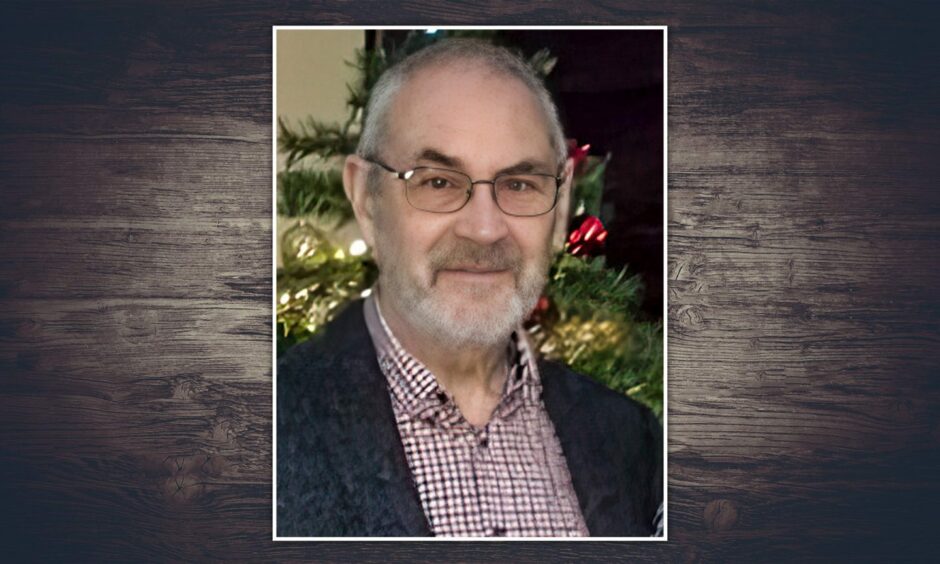
Mary Green’s husband Ralph was looked after in the palliative care ward at Queen Margaret Hospital in his final days last year.
She had spent two months caring for the 76-year-old at home until the strain became too much.
“There is a lot of emphasis on getting people home but it wasn’t as I imagined it would be,” she said.
“In the end I just said, I can’t cope with this.”
The future of palliative care across Fife is under review.
And while NHS chiefs insist no final decisions have been made, the Dunfermline hospice is closed.
Mary said: “It’s a very sensitive subject and people don’t like to complain about the NHS, especially now.
“But there has to be some money somewhere for addressing these issues for the community, not just the NHS.”
‘I thought there would be more physical assistance’
Ralph began end-of-life care in March last year and some adaptations were made to the couple’s Markinch home.
And while nurses and other staff were regularly on hand to help the former policeman, they were not there all the time.
This meant Mary often had to leave him on his own while she ran errands.
“I was at the chemist every day for changes to his medication,” she said.
“I had to leave him all the time. He was not, at that stage, debilitated but when he did move he was definitely at risk.
“He used a walking frame and his legs would just go from under him without any warning. I hated leaving him.”
As Ralph’s condition began to worsen, the physical side of his care began to take its toll on Mary.
More than once, she was unable to get him up after he fell going to the toilet.
“One time, if I hadn’t stuck my leg out to break his fall he would have smashed against the wall,” she said.
“I really thought there would be more physical assistance provided.”
‘Home care does not work for everyone’
It was after one such fall that Mary phoned the helpline number she had been given and the father-of-two was admitted to the hospice in Dunfermline.
“Ralph was six foot two and 14 stone and it was taking two staff to lift him using a hoist,” she said. “How could I do that myself?
“Home care is wonderful for some people but it does not work for everyone.”
Ralph was looked after at Queen Margaret, with a family member by his side, until he died in May.
The closest hospice to Markinch is Kirkcaldy but it was closed for refurbishment at the time, which meant a longer journey for Mary.
“It was quite a lot of travelling each day,” she said.
“For someone in Dunfermline having to do that to Kirkcaldy, I wouldn’t wish it on them.
“There’s enough stress with wondering what you’re going to see, how things have deteriorated, as well as coping with things at home.
“For someone without a car, how would they do that with public transport?
“There has to be a hospice at either end of the county.”
Ongoing review on the future of in-patient hospice care
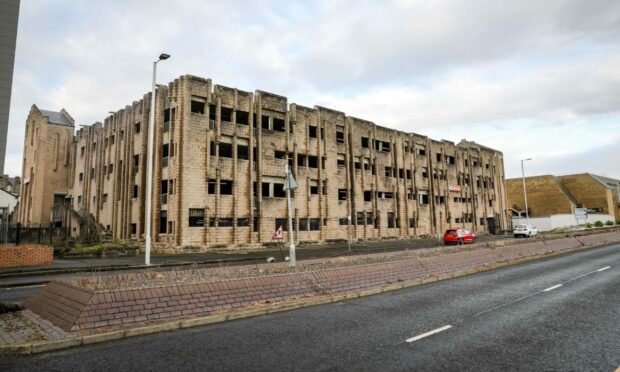
The Dunfermline hospice closed three years ago at the start of the Covid pandemic, with NHS Fife saying they had to protect the most vulnerable patients.
They said the closure was temporary but it has never reopened, apart from a few months last year while the Kirkcaldy hospice was refurbished.
Health chiefs say there has been a sustained reduction in demand for in-patient hospice care, with more people opting to be cared for at home.
Work to determine the long-term future of in-patient end-of-life care is ongoing, they said.
And proposals will be put before the board later this year.
Labour MSP Claire Baker has accused NHS Fife of trying to close the Dunfermline hospice by stealth.
She said: “They are not being open and transparent. Services don’t tend to reopen once they’re shut.”











Conversation