The National Health Service could more accurately be described as the ‘National Sickness Service’ because while it treats illness, it does not often deal with the root causes of why the person got ill in the first place.
Professor Pete Mossey, Professor of Craniofacial Development and Associate Dean for Research at Dundee Dental Hospital, said that the emphasis for the future of the under pressure NHS has to be prevention rather than cure,
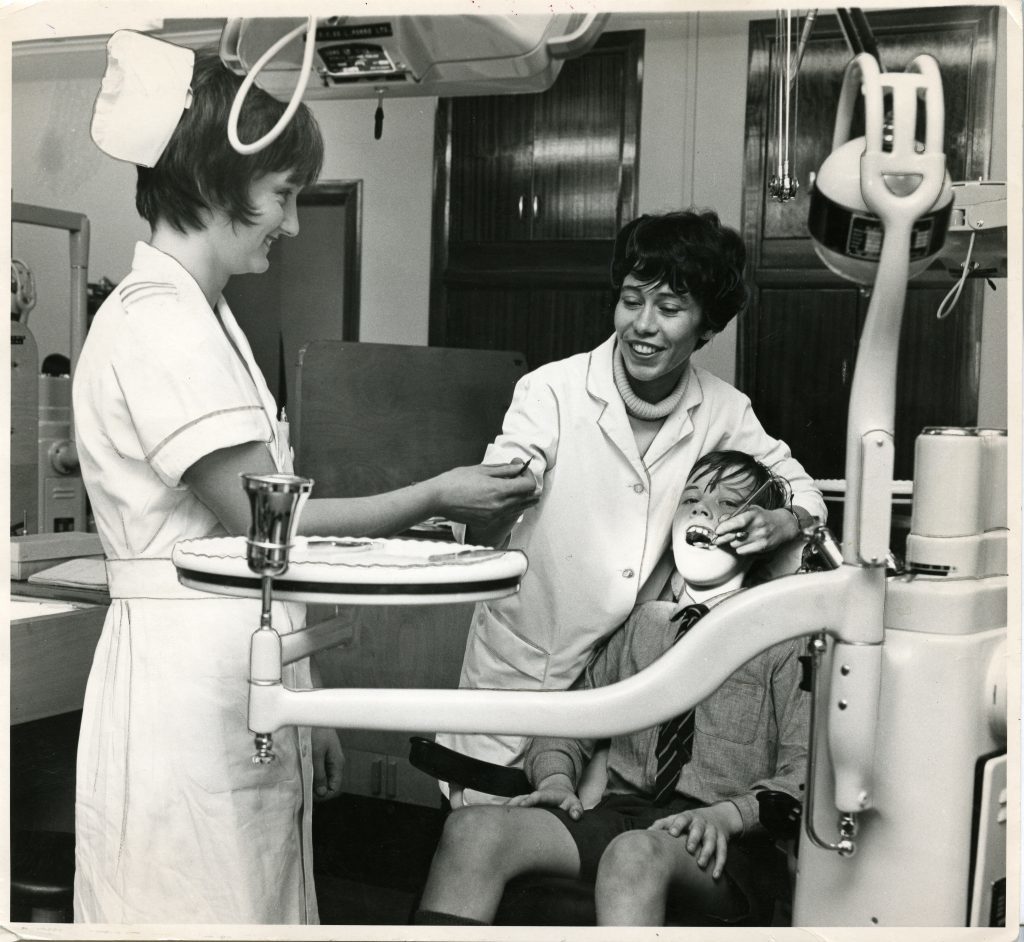
In Scotland tooth extraction is still the number one reason for children receiving general anaesthesia in hospitals.
Statistics show that the trends have a direct relationship to socio-economic status– it’s worse in deprived areas – and Dundee is one of the worst in terms of child hood teeth decay per head of population.
However, Professor Mossey said that while a sugar tax or reduced sugar drinks might seem sensible at face value to reduce obesity, diabetes and improve dental health, it’s a pointless approach unless it is part of a wider, trans-sectoral package of measures designed to improve general health.
The difficulties are that the greatest consumption of sugar per head of population is in deprived areas, and these are often most difficult to reach.
Dundee Dental Hospital has helped Scotland lead on the now globally-recognised Childsmile scheme which is based on the principle of “proportionate universalism”.
The system where the greatest resources go to the areas of greatest need has helped raise the number of caries (decay)-free individuals in Scotland by 20%.
The world renowned Hall Technique was also pioneered at Dundee where instead of drilling cavities a cap is placed on the tooth which seals it off.
However, Professor Mossey believes much more can be done including a ‘Health Coaching’ system being pioneered which focuses on individual responsibility for health.
Instead of providing passive education, dentists engage with the patient and ask them what they are going to do for their own problem.
Meanwhile, technology is being used to remotely diagnosis and treat patients in parts of rural Tayside.
Ian Morrison, 41, consultant neurologist at Ninewells Hospital, explained how instead of patients travelling in to Ninewells from rural Angus or Perthshire, Mr Morrison is now able to carry out consultations via video screens in GP surgeries.
Mr Morrison, who said he “appreciated the NHS far more” after a spell working in America, said: “At our epilepsy clinic about one in three patients don’t turn up for their appointments and that has a significant impact on our clinical workload. That in turn effects our waiting times. So we’ve looked at ways to address that.
“Patients often say they can’t come to hospital, they can’t get to transport, they can’t get their car parked, they don’t feel well enough. If they have psychiatric illness they might feel anxious when they get to hospital. How can we bring the hospital to them? One of the things we looked at was telemedicine.”
Mr Morrison said a study began with the establishment of a telemedicine clinic at Perth Prison. It reflected the difficulties and resources involved in getting prisoners from a secure unit to hospital.
With Tayside being a very diverse geographical area, it also reflected practical issues with using public transport.
“There are also some patients who are very disabled and require significant nursing support where they can’t leave their care home,” he said.
“It’s very difficult for me to go out and practically see them regularly. If people are in their GP surgery, they are more happy to attend because it’s local, a bit different.”