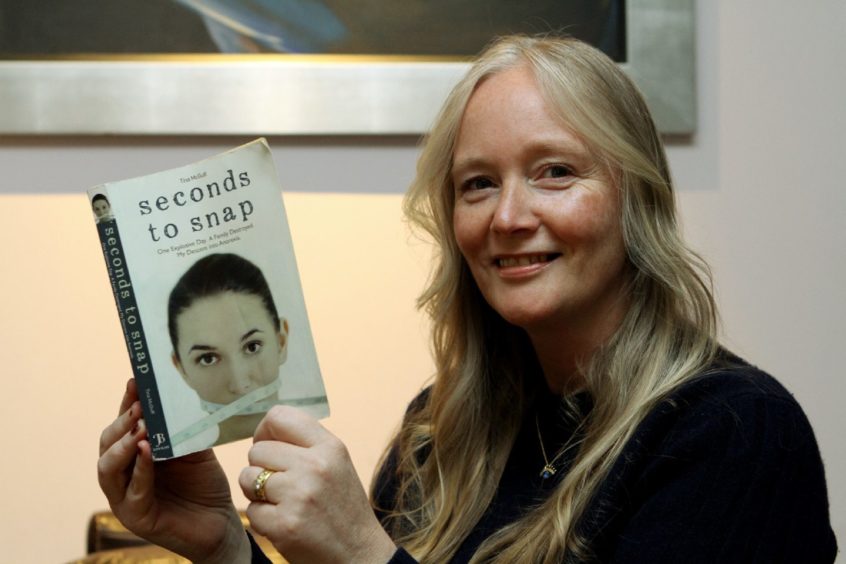
Dundee author Tina McGuff is an anorexia survivor, whose memoir Seconds to Snap, details the years she spent battling the eating disorder and its lasting impact.
Here she writes about her reaction to the death of reality TV star Nikki Grahame, aged 38, after a lifetime battling anorexia, and her hope that the publicity around the tragedy will inspire others to seek, or offer help.
The death of Big Brother star Nikki Grahame is a sad reminder that eating disorders have the highest mortality rates among psychiatric disorders.
In anorexia, this excess mortality is explained in part by the physical complications and in part by an increased rate of suicide. It’s a very complex mental illness.
Anorexia, or any other eating disorder should never be a death sentence, especially in 2021 when we know with evidence-based treatment and early intervention, recovery is always possible, even after many years of illness.
Trauma is universal, as is food, and we use our nervous system to regulate those feelings we feel uncomfortable with.
Anorexia was a shield
For me and many like me anorexia was a shield which I used to stay emotionally safe, without realising it was an addiction and would lead to many years of inpatient therapy.
Now as someone who has now made a full recovery, and from years of working in this this area, I know it’s not always going to be a straightforward journey for everyone.
Nikki Grahame’s death from anorexia has come as a devastating blow to her family, friends and those who loved her, including our community of campaigners and her fans.
Nikki has been very open over the years talking about her battle with anorexia and published her own story Fragile – The true story of my lifelong battle with anorexia then an updated version Dying to be Thin.
She used her platform to raise the public’s awareness of eating disorders, and was never scared to talk about the horrendous reality of living with anorexia; how it stole her childhood, ravaged her body and left her infertile.
Reality was not so glamorous
She used her words to really describe the painful, un-glamourous reality she lived in.
Nikki had been accessing treatment since the age of eight. However, ultimately the NHS couldn’t save her.
And in the months leading up to her death, Nikki’s friends and family had to set up a Go Fund Me page to pay for private specialist care.
Eating disorder treatment services are woefully underfunded, and during lockdown one charity reported a 280% increase in calls in 2020 alone, saying there was concern for sufferers accessing services through their GP.
Often people are turned away because their BMI isn’t low enough, because under-investment means services can only take medically extreme cases.
By the time they have a sufficiently low BMI, they could very well be in need of inpatient treatment, requiring long term care and lessening theirs chance of a full recovery.
Beds and funding fall short
I asked Dr Stephen Anderson, an eating disorder psychiatrist, about available bed space for inpatient treatment in Scotland.
He says there are 26 adult beds available in the NHS and some in general psychiatry. So even if someone needs a bed there is a huge problem accessing one.
Eating disorders affect up to 5% of the population at any point in time, and place an enormous physical, psychological, and financial burden on individuals who are affected and their families.
Just 96p per sufferer is spent on research into eating disorders. For comparison around £9 per sufferer is spent on research into depression
The most recent National Institute for Care Excellence (NICE) guidelines on the recognition and treatment of eating disorders found the evidence-base for both psychological and pharmacological therapies used to treat eating disorders relies on a few small studies, and that many areas remain under-researched.
Here is a figure that may shock you. Just 96p per sufferer is spent on research into eating disorders. For comparison around £9 per sufferer is spent on research into depression.
So what can be done to prevent more people suffering what happened to Nikki Grahame?
Going forward we need much more education right from school age.
When medical students go through university they must be given more than the standard couple of hours on the topic.
Scotland’s Mental Health First Aid strategy needs a section added so all workplaces have this information to share with the workforce.
No one should feel ashamed about struggling with their mental health, especially now as we come out of lockdown
And there are also people like myself who are prepared to deliver workshops across the UK if it means awareness is raised.
Many schools have started teaching mental health qualifications and this can only help to end the stigma that has prevented people from asking for help in the past.
No one should feel ashamed about struggling with their mental health, especially now as we come out of lockdown.
Social media: a curse and a blessing
So many parents ask me about the impact of social media, it’s a dichotomy and a part of the world we now live in.
There are too many appalling accounts promoting unhealthy fad diets. They need to be held accountable, and the platforms need to step up and own that accountability as well as the creators.
However, there are also some amazing, positive accounts on there too, sharing great messages of positivity and hope.
If anyone is concerned about themselves or a loved one, please know you are not alone and there is help available.
Remember early intervention is key, so please ask the question, be there for someone, spot the early warning signs.
A number of sites also provide free information and support, including www.beateatingdisorders.org.uk and the Scottish Eating Disorders Interest Group