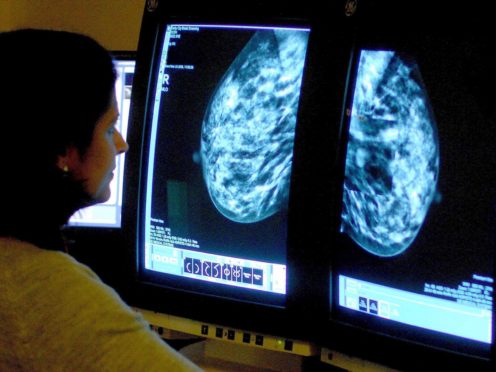
Women who get a “false positive” result following a mammogram are twice as likely to develop breast cancer later in life than those who get a negative result, a study has suggested.
Scientists analysed data from more than a million women in Denmark, Norway and Spain who were screened for breast cancer between 1991 and 2010.
A total of 113,634 women received a false positive result – when apparent abnormalities are found not to be malignant – with the largest proportion occurring in women aged 50-54.
The research, led by Hospital del Mar Medical Research Institute in Barcelona, found those who received one false positive were two times as likely to develop breast cancer compared to those who received a negative result.
The study said: “Most importantly, they remained at an elevated risk over a decade after the false positive result.
“In addition, women who experienced a second false positive result had a four-fold increase in risk.”
The Breast Cancer Now charity said the findings, published in the British Journal of Cancer, could be “really important”.
Chief executive Baroness Delyth Morgan said: “Further investigation is needed, but this study suggests that a ‘false positive’ result may be able to act as a marker for women who could benefit from more frequent screening.
“Crucially, we’d urge women who have received a false positive not to worry unnecessarily about their risk of developing breast cancer – but simply to attend screening when invited, check their breasts regularly and report any unusual changes to their GP.”
She stressed that the link did not show that a false positive itself caused a higher risk of breast cancer, and that further research could help explain why women who receive false positive results may have an increased risk of developing the condition.
“There could be a number of factors involved – for example, screening abnormalities could come as a result of women having a higher breast density, which is known to increase breast cancer risk,” she added.
“Our risk of breast cancer can depend on a combination of our genes, family history, lifestyle, reproductive history and breast density.
“While there is much more research to be done, we are hopeful that tailoring screening to a woman’s individual risk could one day help detect more cases earlier, while enabling those at particularly low risk to avoid unnecessary screening.”